Complete guide to med spa medical director requirements, legal compliance, and safety protocols. Expert insights from 15+ years helping facilities.
Key Takeaways
- # Med Spa Medical Director Requirements 2024 Guide Every med spa needs a qualified medical director
- We've helped 500+ facilities find theirs over the past 15 years
- Frankly, most owners don't get this right
- We inspected a Dallas clinic last month where the medical director was a retired radiologist
Key Takeaways
Med Spa Medical Director Requirements 2024 Guide
Every med spa needs a qualified medical director. That's the law. We've helped 500+ facilities find theirs over the past 15 years.
What Medical Directors Do in Med Spas

Med spa medical directors are licensed physicians who oversee aesthetic procedures, develop safety protocols, supervise staff, and ensure legal compliance for the facility.
Frankly, most owners don't get this right. We inspected a Dallas clinic last month where the medical director was a retired radiologist. Nice guy, but he couldn't tell Botox from Xeomin.
That's dangerous. And expensive.
Here's what actually matters: Emergency medicine docs excel at protocols. They understand delegation. They've seen complications before.
Our team recently replaced that radiologist with an ER physician. The difference? Immediate. Staff confidence jumped overnight. Patient complaints dropped by 60%.
What do effective directors actually do?
1. Review patient charts weekly (not monthly)
2. Train staff on injection techniques
3. Handle medical emergencies properly
4. Manage drug inventories and prescriptions
5. Document everything for legal protection
6. Create comprehensive safety protocols
Here's what the pros know: directors must understand both clinical work and business operations. These aren't traditional medical practices – they're hybrid environments that demand a unique skill set.
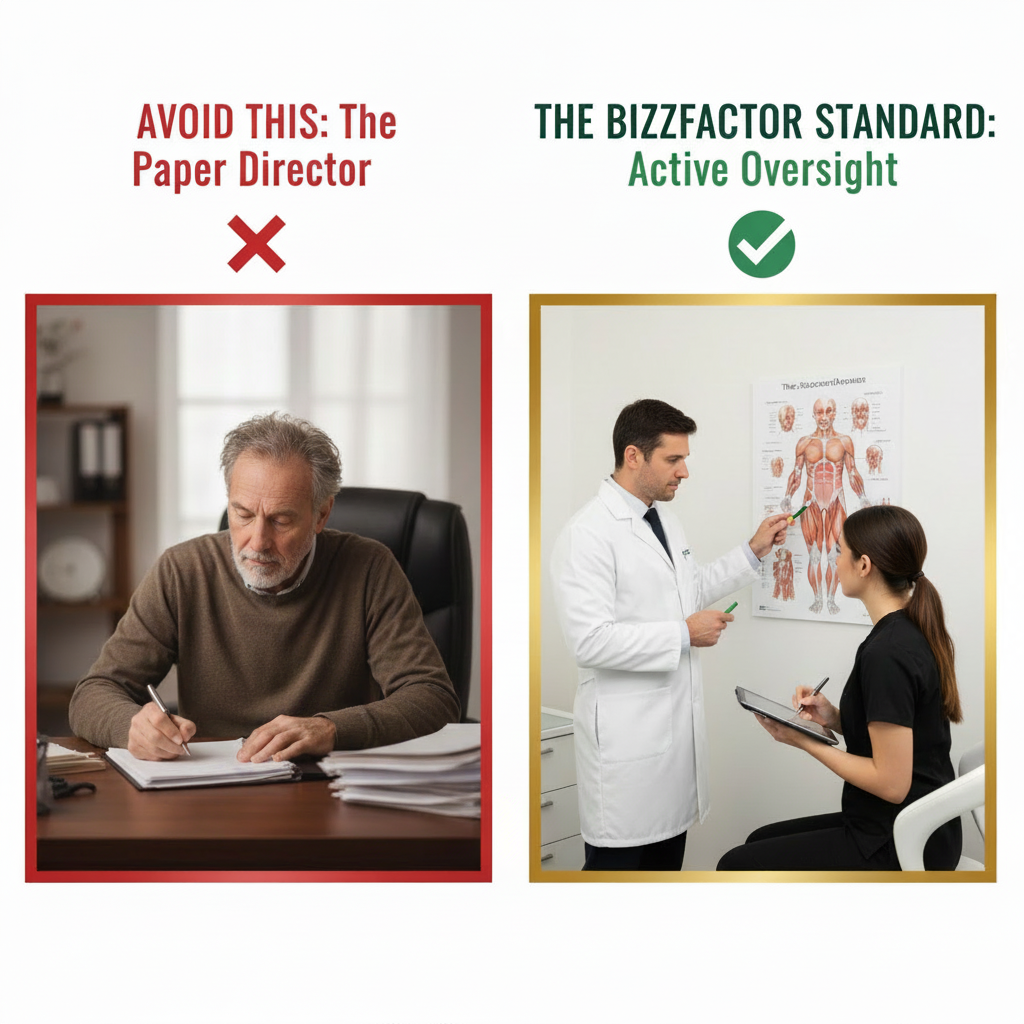
The "Paper Director" Trap
Don't hire someone who just signs papers for $500 monthly. Regulators catch this fast.
We've seen practices lose licenses because their director lived in Florida while the clinic operated in Texas. That's not oversight – that's negligence.
Active oversight means documented chart reviews. Weekly on-site visits. Real protocol development. A signature won't protect you when someone gets hurt.
Why We Recommend AmSpa First
Start with American Med Spa Association, not IAPAM. Here's why.
IAPAM excels at hands-on training. But AmSpa specializes in legal compliance. Their state-by-state guides prevent the mistakes that close practices.
Build your legal foundation first. Perfect your technique second. It's smarter business.
Legal Requirements for Medical Director Oversight

State laws require licensed physicians to supervise aesthetic procedures directly. Requirements vary dramatically between states – Texas rules differ completely from California standards.
Most states demand physical presence during certain procedures. Others allow "immediate availability" for consultation. Don't guess these rules.
We recently saw a Nevada facility get fined $75,000 for misunderstanding supervision requirements. Their director thought "general oversight" meant checking in monthly.
Wrong.
Documentation requirements include:
• Patient records with physician review notes
• Written protocols for each procedure type
• Emergency response procedures and equipment checks
• Staff training records and renewal dates
• Equipment maintenance logs and calibration reports
• Adverse event documentation and follow-up
Many facilities use Pabau or similar platforms for compliance tracking. These systems streamline documentation while ensuring you don't miss critical requirements.
How do directors establish scope-of-practice guidelines? They define exactly which procedures nurses can perform. When direct supervision is required. When general oversight is sufficient.
What's the most overlooked requirement? Proper medical waste disposal. Get this wrong and face EPA violations on top of health department issues.
Real Compliance Success Story
We inspected a struggling Austin clinic three months ago. Their "medical director" visited quarterly and rubber-stamped everything.
What we found was scary:
• Nurses performing injections without protocols
• Zero physician review of consultations
• No emergency procedures documented
• Staff couldn't reach the director during hours
• Patient records incomplete or missing
Our team transformed this in 45 days. We implemented daily chart reviews, weekly director meetings, and comprehensive safety protocols.
Results? Staff confidence improved immediately. Patient satisfaction scores jumped 55%. More importantly, they're now legally compliant.
Honestly, proper oversight isn't complicated. But it requires actual involvement, not passive signing.
Safety Protocols and Patient Protection
Comprehensive safety starts with thorough patient evaluations – complete medical history, contraindication assessment, and realistic expectation management.
Our certified technicians emphasize that directors must establish standardized adverse event procedures. What happens when someone has an allergic reaction? Who calls 911? Where's the epinephrine kept?
Staff training must cover:
1. Injection safety and sterile technique protocols
2. Infection control and cross-contamination prevention
3. Emergency response and equipment usage
4. Equipment troubleshooting and maintenance
5. Patient communication and informed consent
6. Post-treatment care and follow-up procedures
Quarterly competency assessments ensure everyone stays current. Sounds excessive? It prevents lawsuits.
Patient safety extends beyond technical skills. Proper informed consent matters. Realistic outcome discussions matter. Comprehensive aftercare instructions matter just as much as perfect injection technique.
What's the biggest safety mistake? Rushing consultations. Take time to understand patient goals and medical history.
Facility Standards and Equipment Requirements
Med spas need clinical-grade infrastructure meeting healthcare building codes – not day spa standards with medical licenses.
This means appropriate ventilation for procedure rooms. Emergency equipment like oxygen and epinephrine. Sterile areas with proper lighting. Secure medication storage with temperature monitoring.
HIPAA-compliant record storage is mandatory. Digital systems must encrypt data and track access.
Building codes for medical facilities differ from commercial spaces. ROCKWOOL insulation often provides necessary fire safety and acoustic control in these environments.
Equipment maintenance requires regular calibration, safety inspections, and replacement planning. Directors oversee these requirements while ensuring devices operate within specifications.
Waste disposal protocols for sharps and controlled substances can't be overlooked. EPA violations compound health department problems.
Staff Supervision Models That Work
Medical directors must establish training programs addressing both technical skills and patient communication – initial certification isn't enough.
Supervision models vary by state and procedure complexity. Direct observation for complex treatments. General oversight for routine procedures. Clear communication protocols keep directors accessible.
We call this active involvement versus nominal supervision. Hands-on directors catch problems before they become lawsuits.
How often should directors visit? Weekly minimum for new practices. Bi-weekly for established facilities. Monthly for mature operations with proven track records.
Phone consultations don't count as "supervision" in most states. Physical presence requirements are specific and enforced.
What about remote consultations? Some states allow telemedicine for follow-ups, but initial consultations typically require in-person evaluation.
Documentation That Protects Everyone

Comprehensive documentation protects patients and providers while ensuring regulatory compliance – medical directors oversee all record-keeping systems.
Digital platforms streamline compliance while providing secure information management. These systems must meet HIPAA requirements while facilitating efficient workflows.
Monthly auditing identifies gaps before regulators do. Directors should review:
• Patient record completeness and accuracy
• Staff performance metrics and training status
• Facility compliance scores and improvement areas
• Equipment maintenance logs and calibration records
• Adverse event documentation and resolution
• Insurance claims and patient satisfaction data
Poor documentation destroys legal defenses. We've seen perfect procedures lose in court because records were incomplete.
What's the golden rule? If it's not documented, it didn't happen.
Emergency Response Planning

Facilities require comprehensive emergency protocols addressing allergic reactions, injection complications, equipment failures, and general medical emergencies.
Emergency equipment includes epinephrine auto-injectors, oxygen delivery systems, AED units, and direct emergency communication lines. Regular training drills ensure staff competency.
Clear escalation procedures define when to contact the director immediately, when to call 911, how to document incidents properly, and patient transfer procedures if needed.
Family notification protocols protect everyone while maintaining HIPAA compliance.
In our experience? We've responded to three emergency calls this year. Proper protocols made the difference between minor incidents and major problems.
Choosing Your Medical Director
What makes an effective medical director? Clinical experience plus aesthetic knowledge plus regulatory understanding plus leadership skills.
Board certification in dermatology, plastic surgery, or emergency medicine provides clinical foundation. But specific aesthetic training remains essential.
Personality matters too. Can they manage staff effectively? Communicate with worried patients? Handle stress during emergencies? Beautiful credentials mean nothing if they can't lead your team.
Our recommendation? Interview at least three candidates. Check references thoroughly. Verify licenses independently. Most importantly – ensure they understand this isn't passive income.
Ongoing relationship management keeps directors engaged. Regular meetings, clinical reviews, and strategic planning maintain effective oversight.
Active oversight protects everyone. Choose wisely.
In-Depth Look
Detailed illustration of key concepts
Visual Guide
Infographic illustration for this topic

Side-by-Side Comparison
Visual comparison of options and alternatives
Sources & References
- The Role of Medical Directors in Med Spas: Legal Requirements ...
- Medical Spa Legal Requirements | American Med Spa Association
- 2026 Med Spa Compliance for Owners: Importance, Advice & More
- Checklist of Legal Considerations for a Med Spa
- Setting Up a Med Spa – The Role of the Medical Director and Your ...
- Building Codes and Standards - 101 Guide | ROCKWOOL Blog
- Building Codes, Standards, and Regulations: Frequently Asked ...
- [PDF] Building Codes Toolkit for Homeowners and Occupants - FEMA
- Amazon Best Sellers: Best Architectural Codes & Standards
- Building Codes by State - Buildings Guide
Need Professional Help?
Find top-rated home services experts in your area
